In this extract from Print Shift, our one-off publication about 3D printing, editor Claire Barrett reports on the growing number of medical applications for the emerging technology and asks how soon we can expect 3D-printed organ transplants.
Imagine printing a human liver. Or a kidney. One day this will be possible, and with a desperate global shortage of organs for transplant, the medical industry is pouring resources into developing technologies that will make this a reality.
"Eighteen people die every day in the US waiting for a transplant," says Michael Renard, executive vice president for commercial operations at San Diego-based Organovo, one of the companies that is leading the way in tissue engineering.
There is a huge amount of excitement around the potential for printing human tissue. Dr Anthony Atala, director at North Carolina's Wake Forest Institute of Regenerative Medicine, received a standing ovation at a 2011 TED talk where he printed a prototype human kidney live on stage using living cells. Although a fully functioning kidney for transplant is many years away, Atala's primitive organ produces a urine-like substance.
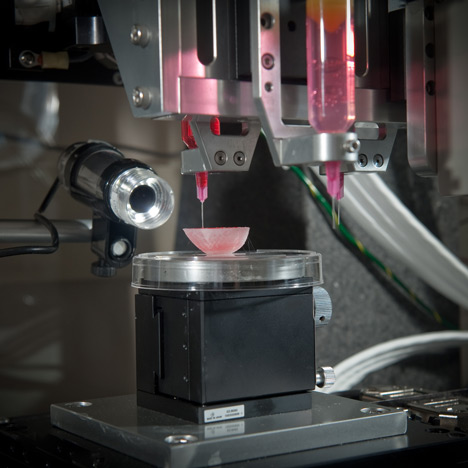
Like other forms of 3D printing, living tissue is printed layer by layer. First a layer of cells is laid down by the printer, followed by a layer of hydrogel that operates as a scaffold material; then the process repeats. The cells fuse, and the hydrogel is removed to create a piece of material made entirely of human cells. This is then moved to a bioreactor, where the tissue continues to grow – as it would in nature – into its final form.
"Our approach is consistent with other forms of 3D printing because it's an additive process," says Renard, "but what is unique is our application of the process in the field of cell biology and tissue engineering."
Currently it is possible to print small pieces of tissue; the problem lies in scaling this and creating a vascular system that delivers oxygen to the cells and removes carbon dioxide. Without this, the cells will die.
In reality, printed organs are a long way away. "In the next 10 years it is possible that [printed] supplemental tissues, ones that aid in regeneration – such as nerve grafts, patches to assist a heart condition, blood vessel segments or cartilage for a degenerating joint – will make it to the clinic," says Renard. "But more advanced replacement tissues will most likely be in 20 years or more."
However, scientists believe that strips of printed tissue will soon be advanced enough to be used to test new drugs. These risk-free tests will help determine whether drugs should move forward to expensive human clinical trials.
Alongside human tissue, 3D printing is being used to develop body parts. In February, Cornell University in Ithaca, New York, announced it had used 3D printing to create an artificial ear for treating a congenital deformity called microtia, where the ear is underdeveloped, or for those who'd lost part of an ear to cancer or an accident.
An alternative to painful rib grafts, which result in ears that neither function well nor look natural, a normal ear is scanned and a mould made by a 3D printer. Collagen is injected into the mould, which acts as a scaffold in the formation of cartilage. The hope is that human trials could take place within three years.
Although this work is headline-grabbing, 3D printing is already common within the healthcare realm. It is used to custom-print hearing aids, and as an alternative to fixed dental braces. Every day, Invisalign – a company that offers a 3D-printed alternative to fixed braces – prints 60,000 sets of transparent custom-made moulds that the wearer changes every two weeks to realign the teeth.
Additive manufacturing is also being used as a visualisation tool to pre-plan surgery. For instance, a heart or fractured leg bone can be scanned and printed to allow the surgeon to intimately understand the anatomy before performing an operation. Surgeons today are using bespoke printed drill and saw guides, which, once the body is opened up, are dropped into place to ensure accurate orientation of the drill in such procedures as hip or knee replacements.
More dramatically, additive manufacturing was used in 2011 to create an entirely new lower jaw for an 83-year-old woman whose own was destroyed by a chronic infection and who was considered too old to sustain reconstructive surgery. Printed in titanium powder by Dutch company LayerWise and only a third heavier than the original, it was covered in bioceramic, a material that ensures the body doesn't reject the implant. Cavities in the printed jaw allowed for muscle reattachment and grooves for the regrowth of nerves.
3D printing has been used for pioneering work within foetal medicine, too. In 2009, Brazilian designer and Royal College of Art PhD student Jorge Lopes introduced the use of 3D printing to create models of unborn children within the womb. Lopes used MRI scans "to see inside the belly of a pregnant woman," he says.
These 3D-printed models are now commonly used to help explain foetal abnormalities to parents, or necessary surgical procedures once the child is born. Most recently Lopes printed out a 3D model of an unborn child for two visually impaired parents who were unable to see their child through regular ultrasound imagery. "It was a very emotional moment," he says.
Inevitably such technologies will reach the mainstream. Since last year, Japanese 3D-printing company Fasotec has offered its Shape of an Angel service to expectant parents at a Toyko clinic. For 100,000 yen parents can receive a 3D-printed model of the foetus inside the womb. The mother's body is printed in clear resin, with the foetus in white.
3D printing also has huge potential to help disability. Magic Arms is shortlisted for the Design Museum’s Design of the Year 2013, and enables Emma Lavelle, a child born with arthrogryposis, to use her arms, a function that was previously impossible. Magic Arms is Emma’s nickname for the Wilmington Robotic Exoskeleton (WREX), an assistive device made up of a bespoke butterfly-patterned jacket and arms that are 3D-printed in durable ABS plastic.
The design was originally made with CNC technology for patients older than two-year-old Emma, but 3D printing enabled it to be translated into a smaller version that is light enough for Emma to wear and take everywhere. If a piece breaks, her mother can simply photograph the broken element and a new one is printed out and sent through the post.
The technology is similarly revolutionising prosthetics. The manufacturer Bespoke Innovations produces Fairings, a 3D-printed covering that can be personalised and worn around the existing prosthetic. Typically a prosthetic will exist either as naked hardware – essentially a pipe – or covered with foam in an attempt to match skin tone and tissue density. "This is the first time there’s been a third option," says founder and industrial designer Scott Summit.
The sound leg is 3D-scanned to ensure body symmetry, and a customised design is 3D-printed to achieve the basic Fairing. This can then be wrapped in different materials such as leather, which can be laser tattooed, and parts can be coated in metal to achieve a final bespoke design that the owner is proud to wear. "The Fairing is just a way that somebody might message to the world, 'Hey, look, it's fine,'" he says.
The greatest benefit of putting 3D printing and 3D scanning together is "that you can start getting rid of the one-size-fits-all mentality," says Summit. While a "small, medium, large universe", as Summit prefers to call it, is perfectly fine for the most part, when you have specific needs – such as a prosthetic limb or a bone defect – the opportunity to personalise your healthcare is tremendous. At a time when healthcare is moving away from the standardised model that developed after the Second World War, 3D printing looks set to be right at the heart of this revolution.